Table of Contents
- Introduction
- Dietary Folate Sources
- Folates in Human Nutrition
- Dietary Reference Intake Standards
- Bioavailability of Folates in Foods
- Folate Concentrations in Serum, Whole Blood, and Cerebrospinal Fluid (CSF)
- Take Home Messages
- Summary and Conclusions
- Did You Know About Folate Receptor Autoantibodies (FRAAs) and Brain Development?
- References
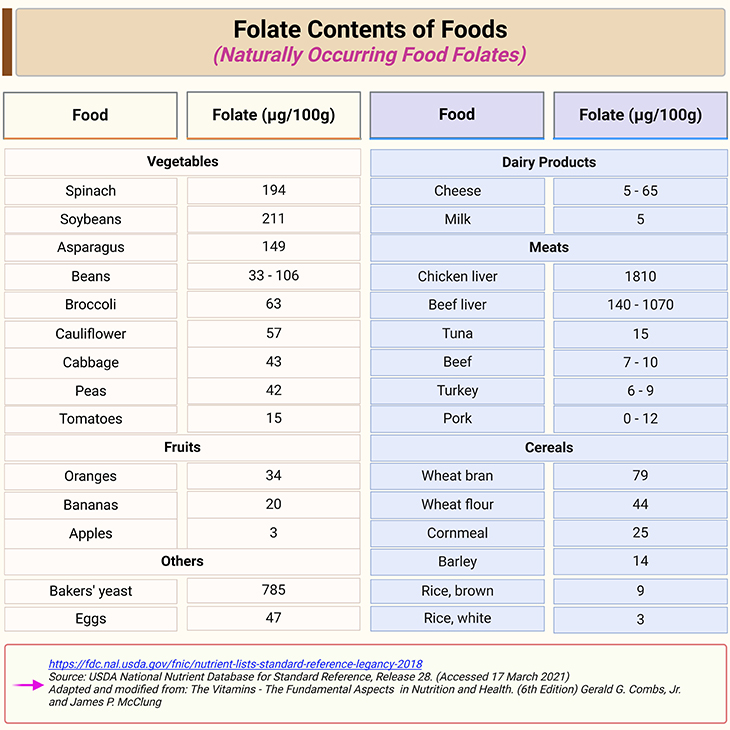
Table 1. Folate contents of foods. A relatively small number of foods are concentrated sources of naturally occurring folate (i.e., food folate); including dark green vegetables, orange juice, legumes, nuts and seeds. Meat is not a nutrient-dense source of folate, except for liver. Substantial losses of this vitamin can occur during the cooking process as a result of the combination of thermal degradation and leaching into the cooking water.
Introduction
Dietary Folate Sources
- Naturally occurring food folate: A relatively small number of foods are concentrated sources of naturally occurring folate (i.e., food folate); including dark green vegetables, orange juice, legumes, nuts and seeds. Meat is not a nutrient-dense source of folate, except for liver (see Table1). Substantial losses of this vitamin can occur during the cooking process as a result of the combination of thermal degradation and leaching into the cooking water [1].
- Folic acid (FA) in fortified foods: FA is added to food in the United States as result of two Food and Drug Administration (FDA) regulations: (1) mandatory fortification of enriched cereal grain products through a standard of identity regulation at 1.4 mg/kg flour or cereal grain product; and (2) optional fortification of ready-to-eat (RTE) products such as breakfast cereals with up to 400 μg of FA/serving through a food additive regulation.
The mandatory FA fortification of enriched cereal grain products beginning in the late 1990s in the United States and Canada has increased the folate content of stable foods such as bread, rice, and pasta, as well as thousands of mixed food items [2].
In addition to enriched cereal grain products, fortified RTE cereals are another important dietary source of FA with the majority of products providing 100 μg/serving and many contributing an amount comparable to the dosage found in supplements, i.e., 400 μg/serving.
FA is also an ingredient in meal replacement foods, infant formulas, and an every-growing number of snack food items such as ‘nutrient bars.’
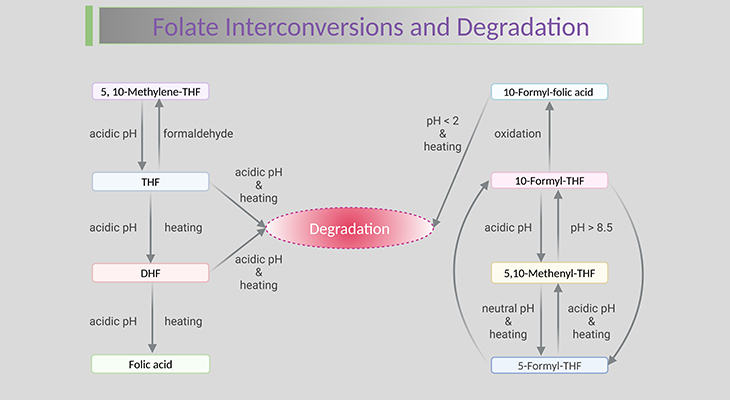
FA was selected as the form of the vitamin used for food fortification because of its excellent stability characteristics. The retention of FA in vitamin-mineral premixes used for food fortification and in RTE cereals has been examined with evidence of little or no loss during storage for up to 6 months, and FA stability during baking of bread products has been reported to be high.
Folates in Human Nutrition
Sources of food folates in human diet are leafy vegetables, liver, wheat germ, and yeast. The main dietary folate forms are (a) 5-methyl-THF and (b) formyl-THF in poly glutamate forms. Folates enter the circulation after absorption in the small intestine (see Figure 1; Table 1).
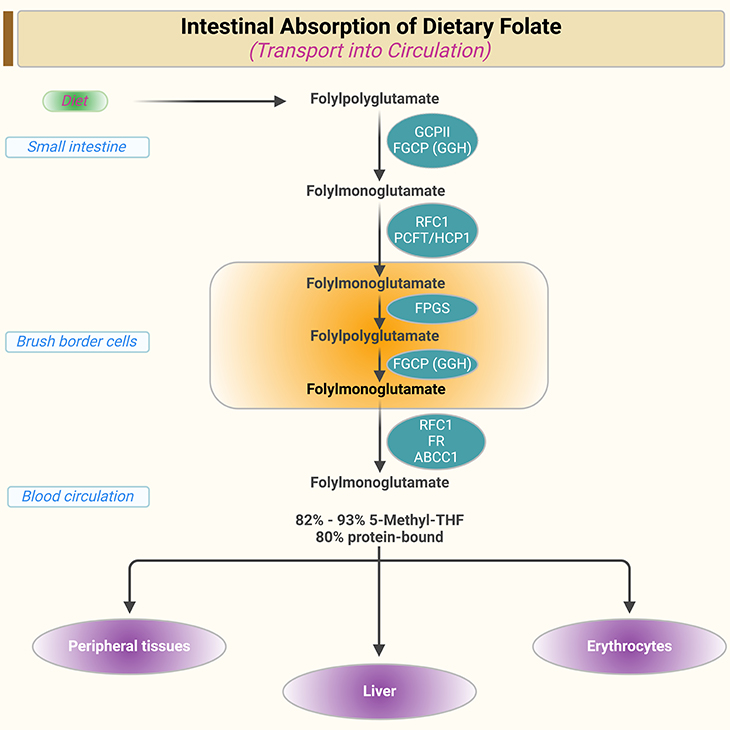
Figure 1. Intestinal absorption of dietary folate and transport into circulation. [ABCC1, ATP-binding cassette, subfamily C, member 1; FGCP, folyl-γ-polyglutamate carboxypeptidase; FPGS, folylpoly-γ-glutamate synthase; FR, folate receptor; GGH, γ-glutamate hydrolase; PCFT/HCP1, proton-coupled folate transporter/heme carrier protein 1; RFC1, reduced folate carrier 1]
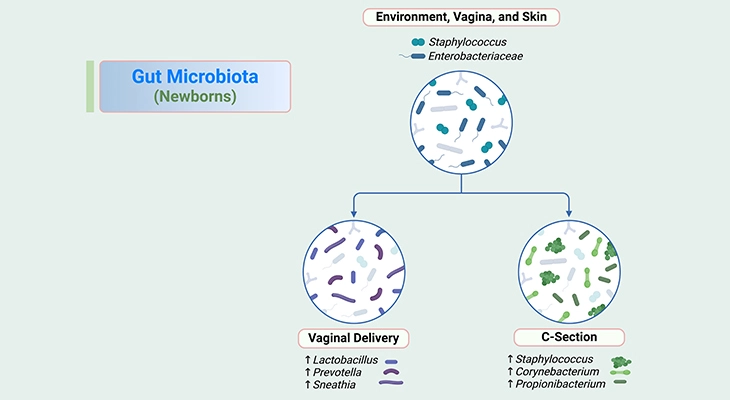
In addition to folates supplied by the diet, folates can be synthesized by the microflora of the large intestine. These folates can be absorbed in the large intestine and were believed to be insignificant for vitamin supply. However, recent studies revealed that the amount of folate absorbed in the colon can cover 5% of the average folate requirements for healthy adults; and can therefore influence the folate status.
The bioavailability of natural folate depends on, for instance:
- the intestinal deconjugation of the polyglutamates,
- the food matrix,
- the stability of the folate forms, and
- the presence of other food constituents that may influence folate stability, for example, ascorbic acid and salts.
The bioavailability of polyglutamates is ~ 65 to 70% lower than that of folate monoglutamates [3].
For more detailed description of intestinal absorption of dietary folate and transport into circulation: (cf. previous blogs entitled as: (i) ‘Folate Transport Systems – I: Transmembrane Carriers,’ (ii) ‘Folate Transport Systems – II: Folate Receptors,’ (iii) ‘Intestinal Absorption of Dietary Folates,’ (iv) ‘Folate Homeostasis and Tissue Accumulation: What You Need to Know.’ ).
Dietary Reference Intake Standards
The Recommended Dietary Allowance (RDA) which were set by the U.S. Institute of Medicine, represents the average daily intake that is sufficient to meet the nutrient requirements of nearly all (97 – 98%) healthy individuals in each age and gender group (see Table 2).
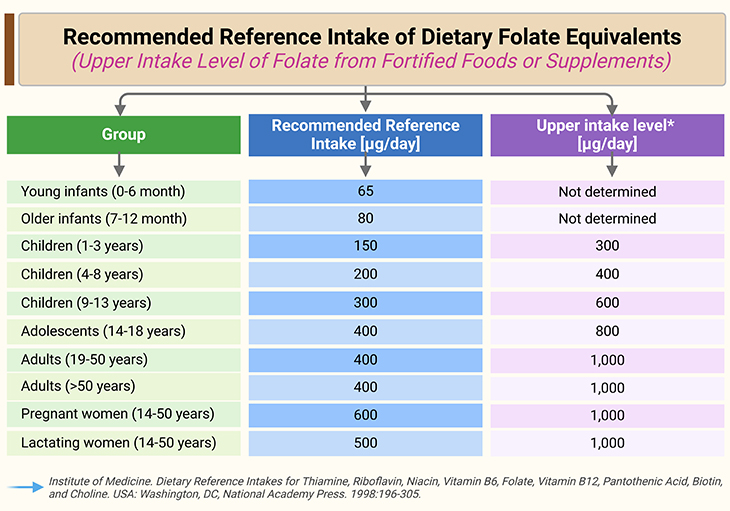
Table 2. Recommended reference intake of dietary folate equivalents and upper intake of folate from fortified foods or supplements by the U.S. Institute of Medicine. *: Upper intake level = 800 μg/day for 14-18 years and 1,000 μg/day for adults.
The recommendation for food folate was based on the assumption that the bioavailability of food folates is no more than 50% of that of FA. The RDA for folate is:
- 400 μg of dietary folate equivalents (DFE)/day for adult males and females,
- 600 μg/day for pregnant women, and
- 500 μg/day for lactating women.
1 μg of DFE is defined as 0.6 μg FA. The upper tolerable limit (UL) for synthetic FA for adults is 1000 μg/day. There is currently little, if any evidence that high intake of natural folates can be harmful to human.
Bioavailability of Folates in Foods
The biological availability of folate in foods has been difficult to assess. Several key factors can affect the utilization of food folates, for instance:
- antifolates that bind to the food matrices, or inhibit the intestinal brush border folyl conjugase;
- inherent differences in folyl glutamates; and
- nutritional status of the host, for e.g., deficiencies of vitamin C and iron can impair the utilization of dietary folate. Vitamin C enhances the utilization of 5-methyl-THF by preventing its oxidative degradation to 5-methyl-DHF, which does not enter the folate metabolic pool.
Interaction of these factors complicate the task of predicting the bioavailability of dietary folates. This problem is exacerbated by methodological difficulties in evaluating folate utilization, which has been approached with bioassays with animal models, and with studies in humans, such as:
- using erythrocyte folate response,
- dilution of stable isotope-labeled folate, or
- urinary folate excretions.
Each has limitations. The result is that estimates of the bioavailability of folates in foods and mixed diets are highly variable (see Table 3) [4].
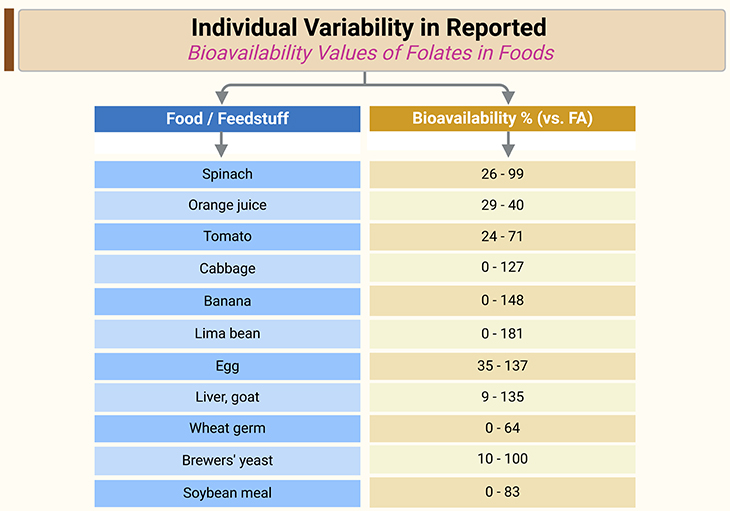
Table 3. Individual variability in reported bioavailability values of folates in foods. [FA, folic acid]
[Sources: Tamura T, Stokstad EL. The availability of food folate in man. Br J Haematol. 1973 Oct;25(4):513-32.; Babu S, Srikantia SG. Availability of folates from some foods. Am J Clin Nutr. 1976 Apr;29(4):376-9.; Baker H, Jaslow SP, Frank O. Severe impairment of dietary folate utilization in the elderly. J Am Geriatr Soc. 1978 May;26(5):218-21.]
Folate Concentrations in Serum, Whole Blood, and Cerebrospinal Fluid (CSF)
Serum concentration of folates ranges between ~ 10 – 50 nmol/L, with 5-methyl-THF predominating (82 – 93% of total folate serum). Most of the blood folate is unspecifically bound to proteins [e.g., α2-macroglobulin, albumin (Kd ~ 1 mmol/L), and transferrin] with a low affinity.
Folate-binding proteins (FBPs) bind a small amount of blood folate with high affinity (Kd ~ 1 nmol/L). The concentration of FBPs in human serum is approximately 0.6 nmol/L, whereas there is a 10 – 30 fold higher molar concentration of folate in serum. The serum FBPs are fully saturated with folate. The liver is responsible for the maintenance of the serum folate concentration. This is ensured by the reversible formation and depletion of the intracellular non-methylated folate polyglutamates.
The reference values of fasting serum folate concentrations for children, adolescents, and adults are presented in Table 4 (see Table 4) [5].
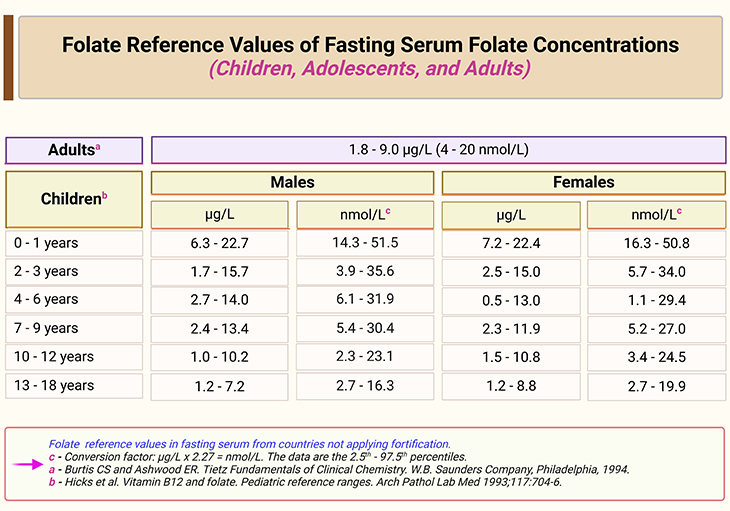
Table 4. Folate reference values in fasting serum from countries not applying fortification. The data are the 25th – 97.5th percentiles. [C, Conversion factor: μg/L x 2.27 = nmol/L]
Folates are incorporated into red blood cells (RBCs) during erythropoiesis. FBPs are expressed on early stage hematopoietic cells and are involved in the folate uptake. The reduced folate carrier (RFC) is necessary for the folate transport in erythroid cells. Folate in erythrocytes are mainly 5-methyl-THF and formyl-THF in their polyglutamate form, mostly penta- and hexaglutamates. Usually, RBC folate is 30 fold higher than the serum folate concentration ranging from 140 – 450 ng/mL packed cells.
Similar to serum, the RBC folates are unspecifically bound to proteins such as hemoglobin. Matured erythrocytes are impermeable for folylpolyglutamates. This leads to an intracellular retention of the folates with a half-life of about 100 days (the lifespan of the erythrocytes, RBCs). Therefore, RBC folate represents a long-term marker for folate status. This maker is not affected by recent changes in the dietary intake.
The 5-methyl-THF and non-methyl-THF concentrations obtained by liquid chromatography-tandem mass spectrometry (LC-MS/MS) methods in serum and EDTA whole blood (WB) are summarized in Table 5 (see Table 5) [6-8].
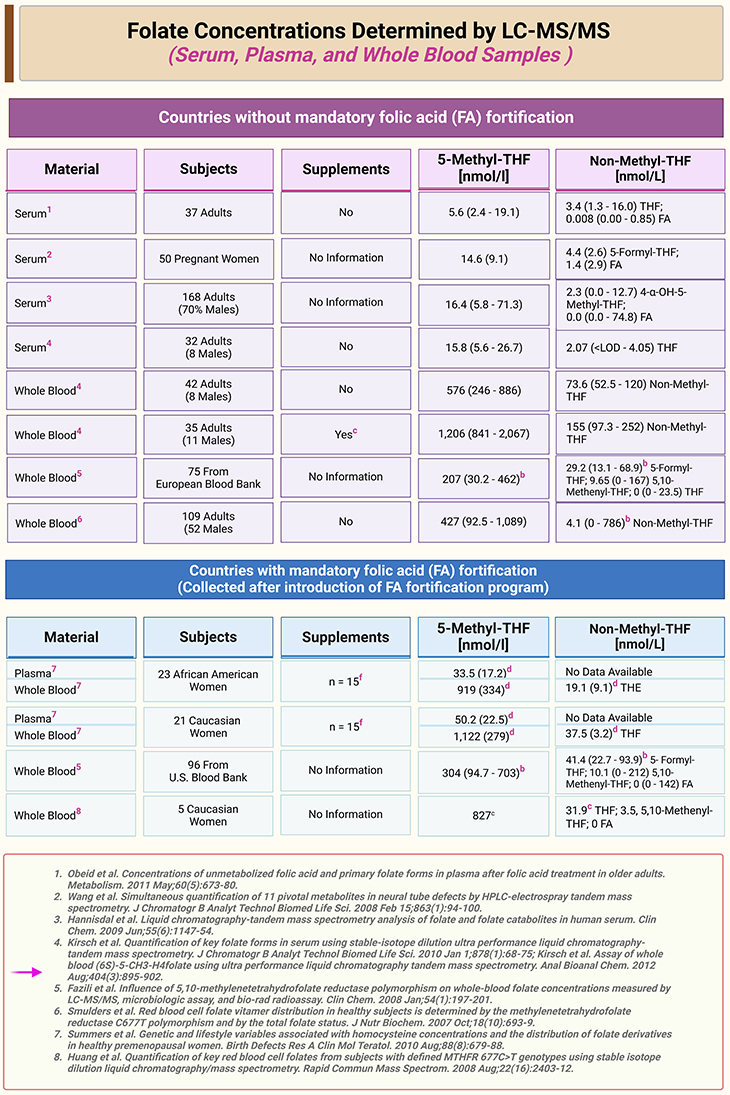
Table 5. Folate concentrations in serum, plasma, whole blood samples determined by LC-MS/MS. The data are presented as medians (10th – 90th percentiles), b: medians (range); d: means (standard deviations, SDs); or e: means concentrations. a: UPLC-MS/MS. c: Supplementation with 500 μg folic acid, 50 mg vitamin B6, and 500 μg B12 for 6 months. f: Supplements included multivitamins, B vitamins, and folic acid. [THF, tetrahydrofolate; FA, folic acid; WB, whole blood; LC-MS/MS, liquid chromatography-tandem mass spectrometry; UPLC-MS/MS, ultra-performance liquid chromatography-tandem mass spectrometry]
The folate transport into the cerebrospinal fluid (CSF) occurs in the choroid plexus, where 5-methyl-THF is transported across the blood-CSF barrier. The membrane folate receptor α (FOLR1/FRα) is the most abundant folate transporter in the choroid plexus, suggesting its role as major folate transporter across the blood-CSF barrier. The recently described proton-coupled folate transporter/heme carrier protein 1 (PCFT/HCP1) functions most likely in concert with the FRα (adult brain) and FRβ (fetal brain) or might export the folates after FRα-mediated endocytosis. The folate concentrations in the CSF are up to 3 times higher than in serum (see Table 6).
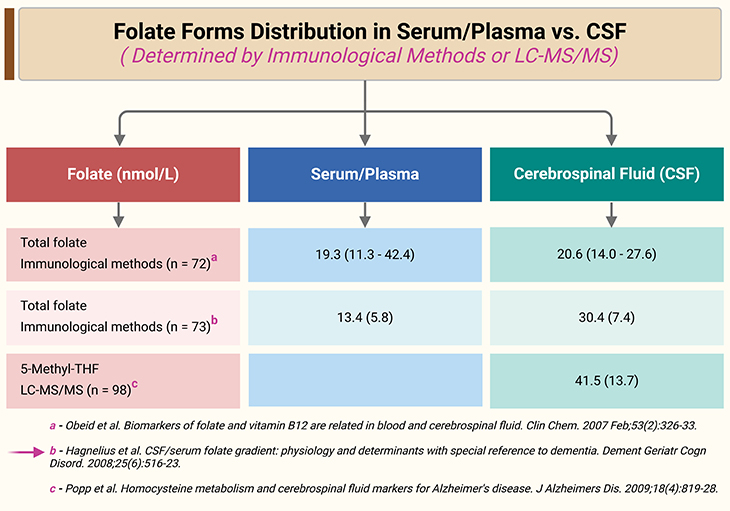
Table 6. Folate forms distribution in serum/plasma and CSF determined by immunological methods or LC-MS/MS. The data are medians (10th – 90th percentile) or means (standard deviation, SD). [THF, tetrahydrofolate, LC-MS/MS, liquid chromatography-tandem mass spectrometry]
The cerebral folate deficiency (CFD) is defined as “a neurological syndrome associated with low CSF concentrations of 5-methyl-THF in the presence of normal peripheral folate status.” CFD has an early onset in late infancy and is characterized by, for example:
- severe developmental disorders,
- mental retardation,
- epilepsy, and
- movement disorders.
CFD can be associated with peripheral folate deficiency, but this might not be case in some cases. In cases with normal peripheral folate status, CFD may develop due to the impaired folate transport across the blood-CSF barrier at the choroid plexus.
Other disease conditions that are associated with CFD are, for example:
- Rett syndrome,
- Kearns-Sayre syndrome,
- Aicardi-Goutiere’s syndrome, and
- Hypomyelination with atrophy of the basal ganglion syndrome.
Oral dose of folinic acid (5-formyl-THF) can normalize the CSF folate and lower the frequency and the severity of the epileptic seizures in affected patients.
Take Home Messages
Sources of Folate
- As its name suggests, the best natural sources of folate are leafy vegetables.
- Two other sources are vital: (i) organ meats, such as chicken and beef liver; and (ii) folic acid-fortified cereal products.
Folate Bioavailability
- Folic acid is absolutely bioavailable as a dietary supplement and highly bioavailable from fortified foods.
- Food folates have bioavailabilites of 10% – 98%; most are ~ 50%.
- Mixed diets have aggregate bioavailabilities of 50% – 80%.
Serum/Whole Blood/CSF Folate
- Serum folates: reflect recent folate intake.
- Erythrocyte folates: reflect longer-term intake and are generally more useful in assessing folate status.
- CSF folates: the folate concentrations in the CSF are up to 3 times higher than in serum.
Summary and Conclusions
In this blog, we have attempted briefly to characterize the magnitude of folate status/deficiencies in the United States and elsewhere. Mainly focusing on folate in human nutrition, dietary sources and bioavailability of folates in foods, and most importantly, folate concentrations in serum, whole blood, and CSF in children, adolescents, and adults.
In general, definite conclusions pertaining to the extent of folate status/deficiencies could not be drawn because of limitations of the data, including: (a) the paucity of population-based studies designed to assess folate status at the national or regional level; (b) variation in the life-stage groups (for e.g., children, pregnant women) evaluated in different countries, with very few surveys designed to assess the folate status in the general population; (c) use of different analytical methods to measure serum and RBC (erythrocyte) folate, which raises concern regarding assay variability and validity, and (d) use of poorly defined and inconsistent cutoff values to define folate deficiency based on serum and/or RBC folate concentrations.
It was possible, however, to provide some indication based on the evaluation of available data that in the majority of countries for which there are national survey data, folate deficiency appears to be a public health problem. This clearly demonstrates that there is a pressing need for further studies to address the limitations of the folate assessment data, which will facilitate planning for appropriate public health intervention strategies in specific countries around the world, including United States!
For information on autism monitoring, screening and testing please read our blog.
References
- Gregory JF 3rd. Chemical and nutritional aspects of folate research: analytical procedures, methods of folate synthesis, stability, and bioavailability of dietary folates. Adv Food Nutr Res. 1989;33:1-101. doi: 10.1016/s1043-4526(08)60126-6. PMID: 2697230.
https://pubmed.ncbi.nlm.nih.gov/2697230/ - Lewis CJ, Crane NT, Wilson DB, Yetley EA. Estimated folate intakes: data updated to reflect food fortification, increased bioavailability, and dietary supplement use. Am J Clin Nutr. 1999 Aug;70(2):198-207. doi: 10.1093/ajcn.70.2.198. PMID: 10426695.https://pubmed.ncbi.nlm.nih.gov/10426695/
- McNulty H, Pentieva K. Folate bioavailability. Proc Nutr Soc. 2004 Nov;63(4):529-36. doi: 10.1079/pns2004383. PMID: 15831124.
https://pubmed.ncbi.nlm.nih.gov/15831124/
- Brouwer IA, van Dusseldorp M, West CE, Steegers-Theunissen RP. Bioavailability and bioefficacy of folate and folic acid in man. Nutr Res Rev. 2001 Dec;14(2):267-94. doi: 10.1079/NRR200126. PMID: 19087427.
https://pubmed.ncbi.nlm.nih.gov/19087427/ - Hicks JM, Cook J, Godwin ID, Soldin SJ. Vitamin B12 and folate. Pediatric reference ranges. Arch Pathol Lab Med. 1993 Jul;117(7):704-6. PMID: 8323433.
https://pubmed.ncbi.nlm.nih.gov/8323433/ - Obeid R, Kostopoulos P, Knapp JP, Kasoha M, Becker G, Fassbender K, Herrmann W. Biomarkers of folate and vitamin B12 are related in blood and cerebrospinal fluid. Clin Chem. 2007 Feb;53(2):326-33. doi: 10.1373/clinchem.2006.076448. Epub 2007 Jan 2. PMID: 17200133.
https://pubmed.ncbi.nlm.nih.gov/17200133/ - Hagnelius NO, Wahlund LO, Nilsson TK. CSF/serum folate gradient: physiology and determinants with special reference to dementia. Dement Geriatr Cogn Disord. 2008;25(6):516-23. doi: 10.1159/000129696. Epub 2008 May 7. PMID: 18463447.
https://pubmed.ncbi.nlm.nih.gov/18463447/ - Popp J, Lewczuk P, Linnebank M, Cvetanovska G, Smulders Y, Kölsch H, Frommann I, Kornhuber J, Maier W, Jessen F. Homocysteine metabolism and cerebrospinal fluid markers for Alzheimer’s disease. J Alzheimers Dis. 2009;18(4):819-28. doi: 10.3233/JAD-2009-1187. PMID: 19661622.
https://pubmed.ncbi.nlm.nih.gov/19661622/