Oftentimes ADHD (Attention-Deficit/Hyperactivity Disorder) and Autism get confused. ADHD and autism can have many overlapping symptoms and it may be difficult for parents and medical professionals to discern the difference between the two.
So, what exactly is ADHD and how is it different than Autism? And how are these conditions similar?
ADHD stands for Attention-Deficit/Hyperactivity Disorder, and it is a neurodevelopmental disorder that affects both children and adults. ADHD is characterized by a persistent pattern of inattention, impulsivity, and hyperactivity that can significantly impair an individual’s daily functioning and quality of life. The symptoms of ADHD fall into the following cluster:
- Inattention: Individuals with ADHD often struggle to focus and sustain attention on tasks or activities that require mental effort. They may make careless mistakes, have difficulty organizing tasks and activities, avoid or procrastinate on tasks that require sustained attention, frequently lose items necessary for tasks, and appear forgetful in daily activities.
- Hyperactivity: Some people with ADHD exhibit hyperactive behavior. This would include restlessness, excessive fidgeting, difficulty remaining seated in situations where it’s expected, and a tendency to be “on the go” as if driven by a continuous motor.
- Impulsivity: Impulsivity refers to acting on urges or impulses without considering the potential consequences. Individuals with ADHD may have trouble waiting their turn, frequently interrupt conversations, and have difficulty with impulse control, which can lead to rash decisions and/or actions.
ADHD is a clinical diagnosis made typically by healthcare professionals based on a comprehensive evaluation of an individual’s symptoms, developmental history, and the exclusion of other potential causes. A person with ADHD will not necessarily exhibit all three categories of symptoms. ADHD, however, is further categorized into three subtypes:
- Predominantly Inattentive Presentation: Characterized primarily by symptoms of inattention, with fewer or no symptoms of hyperactivity-impulsivity.
- Predominantly Hyperactive-Impulsive Presentation: Characterized primarily by symptoms of hyperactivity and impulsivity, with fewer or no symptoms of inattention.
- Combined Presentation: The most common type, which involves a combination of symptoms from both the inattention and hyperactivity-impulsivity categories.
ADHD is one of the most common neurodevelopmental disorders of childhood. It is usually first diagnosed in childhood and often lasts into adulthood. ADHD can have a significant impact on various aspects of an individual’s life, including academic and occupational performance, relationships, and overall well-being. Early diagnosis and appropriate treatment, which may include behavioral therapy, medication, or a combination of both, can help individuals with ADHD manage their symptoms and improve their quality of life.
It is not uncommon for children to have trouble concentrating and behaving at certain points in their lives. However, children with ADHD do not just grow out of these behaviors. It is likely that the symptoms will persist and become severe, causing difficulties at home, at school, and in social situations.
The CDC (Centers for Disease Control and Prevention) lists some actions that fall into the category of ADHD.
A child may:
- daydream a lot
- forget or lose things a lot
- squirm or fidget
- talk too much
- make careless mistakes or take unnecessary risks
- have a hard time resisting temptation
- have trouble taking turns
- have difficulty getting along with others
- Interrupt people or have trouble waiting their turn
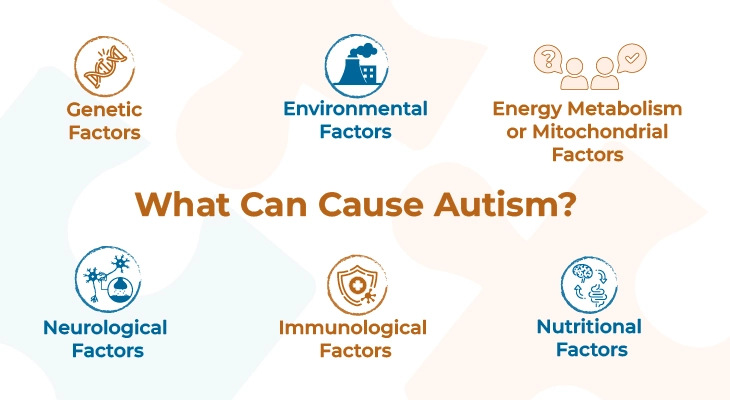
The exact cause of ADHD is not fully understood, but it is believed to result from a complex interplay of genetic, environmental, and neurological factors. Here are some key factors that are thought to contribute to the development of ADHD:
Genetic Factors: There is a strong genetic component to ADHD. In studies, it has been demonstrated that individuals with a family history of ADHD are more likely to develop the disorder themselves. Specific genes associated with neurotransmitter regulation and brain development are thought to play a role in predisposing individuals to ADHD.
Environmental Factors: While genetics play a significant role, environmental factors can also contribute to the development of ADHD. These factors may include prenatal exposure to toxins (e.g., alcohol or tobacco), premature birth, low birth weight, and lead exposure. Maternal smoking and substance abuse during pregnancy have been associated with an increased risk of ADHD in children.
Brain Injury or Trauma: In some cases, brain injury or trauma to the frontal lobe of the brain can lead to symptoms of ADHD. This is somewhat different to traditional ADHD and is referred to as “acquired” ADHD.
Other: Oftentimes it is mentioned that certain other contributing factors, such as a chaotic or stressful home environment, neglect, early exposure to violence, eating too much sugar, watching too much television, or poor parenting, may contribute to the development or exacerbation of ADHD symptoms in some individuals. These claims are not thoroughly supported by research. Of course, many things, including these, might make symptoms worse, especially in certain people, but again, the evidence is not strong enough to conclude that they are the main causes of ADHD.
Diagnosis:
Diagnosing a child for ADHD is a process involving several steps. There is no single test to diagnose ADHD. The process traditionally begins with a medical exam, including hearing and vision tests, to rule out other problems with similar symptoms to ADHD. Additionally, diagnosing ADHD includes a checklist for rating ADHD symptoms and taking a history of the child from parents, teachers, and sometimes, the child him/herself.
Healthcare professionals use the guidelines in the American Psychiatric Association’s Diagnostic and Statistical Manual, known as DSM-5, to help diagnose ADHD. This diagnostic standard helps ensure that people are appropriately diagnosed and treated for ADHD.
ADHD, Autism, or both?
Symptoms of both autism and ADHD often mirror each other and include inattention, social difficulties, hyperactivity, and impulsivity. While some individuals are diagnosed with either Autism or ADHD, others may be diagnosed with both. A child impacted by one or both conditions can have trouble with their abilities to communicate and focus, especially with social skills. Often, these correlates can lead to confusion between diagnosis and treatment, but it’s important not to lump them together when pursuing treatments that should specifically address each condition.
In many cases, parents, caregivers, and educators make assumptions about a child’s behavior before a diagnosis has been made. Understanding key differences between these disorders can facilitate accurate diagnosis and treatment that will enable a child to succeed.
Similarities between ADHD and Autism:
Some of these similarities are:
- Both are neurodevelopmental disorders that affect the central nervous system
- Both typically involve delayed communication skills, at the onset of development
- Both are diagnosed at a higher rate in boys than in girls
- Both may lead to challenges with understanding/controlling emotions, actions and feelings
- Both may struggle with making and maintaining eye contact
- Both have no “cure”, but are treatable and symptoms may be managed accordingly
Differences between ADHD and Autism:
- Communication is more often delayed in autism whereas communication develops into a mode of hyperactivity in ADHD
- ADHD is more typically developed and diagnosable after the age of 4 (generally); Autism symptoms may be diagnosed at an earlier age
- ADHD symptoms can be effectively managed with prescription medication; Autism is rarely treated with prescription medication
- Children with autism are more often withdrawn or disengaged than those children with ADHD
- Children with autism often struggle in social interactions and may be non-verbal; conversely, children with ADHD may hyperactively talk and attempt to dominate social settings
These are just a few similarities and differences between ADHD and autism. It is important to remember that each child and their condition(s) are different and must be treated uniquely despite common expectations for either disorder.
Can a Person Be Diagnosed with Both ADHD and Autism?
Someone can be diagnosed with both autism and ADHD. A significant number of individuals with autism spectrum disorder (ASD) also present with comorbid ADHD. The combination is more often diagnosed in children than adults, especially as ADHD has symptoms that can dissipate later in life.
ASD is considered a lifelong condition, and a diagnosis of autism often stops a search for further clinical diagnoses. However, it is worth knowing the similarities and differences to avoid misdiagnosing either condition.
How to Diagnose ADHD vs. Autism?
The American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders incorporates three main components of ASD:
The diagnosis of ADHD and ASD often involves the same team of medical professionals, but there are distinct differences in when and how they are diagnosed.
Autism Diagnosis:
Symptoms of autism begin showing anywhere between 12-36 months, and most parents will see some signs of autism before their child turns two years old.
- Impaired communication
- Impaired reciprocal social interaction
- Restricted, repetitive, and stereotyped patterns of behaviors or interests
To properly diagnose autism, you should consult a pediatrician/pediatric neurologist/psychiatrist. From there, the medical professional(s) should be able to perform tests or screenings to make a proper diagnosis.
ADHD Diagnosis:
ADHD symptoms typically appear during elementary school ages for children – around 4-9 years old. The reason for this may be that school environments require focus, organization, and performance based on these attributes, and they have not yet had the chance to display their symptoms as a result.
If you suspect that your child may require an ADHD diagnosis, make a list of possible symptoms, and have the educator document them. Additionally, confirm these with a physician or a specialist, who can then perform observational screenings. Typically, ADHD screenings are performed after six months or more of persisting symptoms.
Treatments for Autism and ADHD:
Although treatment for these two conditions is different, neither is perfectly defined or standard for all. ADHD sometimes relies on prescription medication, whereas prescription medication for autism is largely limited. In many cases, ADHD is treated with a combination of behavior therapy and medication. For preschool-aged children (4-5 years of age) with ADHD, behavior therapy is recommended as the first line of treatment before medication is administered. Treatment plans will often include close monitoring, with follow-up changes if necessary.
Although treatment for these two conditions is different, neither is perfectly defined or standard for all. ADHD sometimes relies on prescription medication, whereas prescription medication for autism is largely limited. In many cases, ADHD is treated with a combination of behavior therapy and medication. For preschool-aged children (4-5 years of age) with ADHD, behavior therapy is recommended as the first line of treatment before medication is administered. Treatment plans will often include close monitoring, with follow-up changes if necessary.
Effective treatment for both conditions requires consistent monitoring and a robust support system to manage the symptoms of ADHD and ASD. This includes proper diagnoses and a strong network of parents, educators, physicians, and specialists who address each case with evidence-based treatment. For autism, treatment is most effective through ABA therapy. As with either condition, early intervention is critical and can play a large part in the success of treatments for the child.
For information on autism monitoring, screening and testing please read our blog.