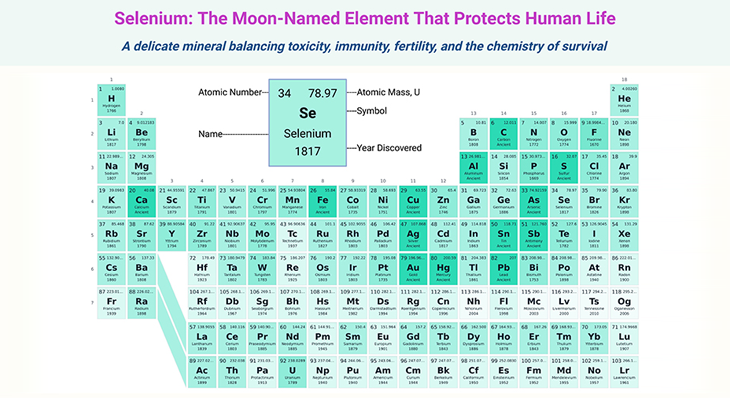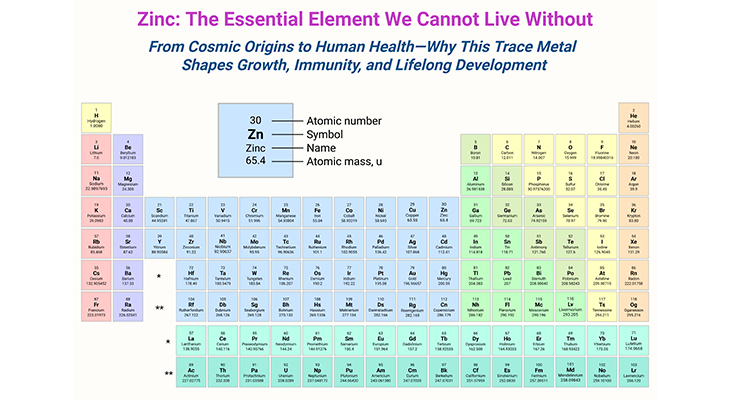
Figure 1. Four Diets, One Brain: Mapping the Menus that Safeguard Cognitive Health. Comparative overview of brain-healthy dietary patterns—Mediterranean, DASH, MIND, and Ketogenic diets—and their key components, proposed mechanisms of action, and neurological relevance. (1) The Mediterranean diet emphasizes high intake of vegetables, fruits, legumes, whole grains, nuts, olive oil, and fish, with limited red meat and sweets. It is rich in anti-inflammatory and antioxidant compounds, including polyphenols and omega-3 fatty acids, and has been associated with reduced risk of depression and Alzheimer’s disease through modulation of oxidative stress and inflammation. (2) The DASH (Dietary Approaches to Stop Hypertension) diet focuses on blood pressure regulation and includes fruits, vegetables, low-fat dairy, whole grains, poultry, fish, and nuts, while minimizing sodium, red meat, and added sugars. It promotes cerebrovascular health and may reduce the risk of cognitive decline by supporting vascular integrity and metabolic homeostasis. (3) The MIND (Mediterranean-DASH Intervention for Neurodegenerative Delay) diet is a hybrid that selectively combines the neuroprotective elements of the Mediterranean and DASH diets. It prioritizes leafy greens, berries, nuts, whole grains, and fish, and discourages butter, cheese, red meat, and fast food. Adherence has been linked to slower cognitive aging and reduced Alzheimer’s risk—even with moderate compliance. (4) The Ketogenic diet, characterized by high fat, very low carbohydrate, and moderate protein intake, induces hepatic ketogenesis and the production of β-hydroxybutyrate. It has been shown to alter neuronal energy metabolism, reduce neuroinflammation, and improve mitochondrial efficiency. Though traditionally used in epilepsy, emerging evidence suggests potential benefits in neurodegenerative and mood disorders, though long-term safety and adherence remain areas of investigation.
Introduction
In an age where depression and dementia are rising with unsettling speed, a quiet revolution is taking root at the dinner table. For decades, the brain was viewed as a biochemical black box—treated with pills, probed with scans, and often misunderstood. But today, a bold new question is reshaping the frontiers of neuroscience and psychiatry: Could the path to a healthier brain begin not in a lab, but in our kitchens?
Emerging from the intersection of nutrition science, evolutionary biology, and clinical psychiatry is a powerful idea—that what we eat can shape how we think, feel, and age. This is not just about eliminating junk food or counting calories; it is about understanding the brain as a nutrient-hungry organ, deeply entwined with the health of our gut, our genes, and even our microbes.
The story you are about to explore is not merely about omega-3s or antioxidants, though they play starring roles. It is about a deeper truth: “food is information”. And the messages we send through our meals can either nurture clarity and calm—or feed inflammation, fog, and despair. This is the dawn of nutritional psychiatry, and it has the potential to transform how we prevent, manage, and even reverse mental illness.
What follows is a journey—from one woman’s transformation to the latest peer-reviewed discoveries—uniting ancient wisdom with modern science to reimagine what it means to eat for the mind.
Rethinking Mental Health—One Bite at a Time
A Personal Awakening – Carolyn’s Journey: When 75-year-old Carolyn, a retired radiology film librarian from Pittsburgh, talks about her lifestyle today, her voice radiates calm and clarity. She exercises regularly, cherishes time with her grandchildren, and maintains strong social ties. But rewind seven years, and the picture looked very different.
Carolyn had just lost her mother. Her two sons had moved away. Burdened by grief, she found herself isolated, slipping into depression, and battling chronic conditions—diabetes, lung disease, and excess weight—while relying heavily on junk food for comfort.
Then came a turning point. Through a friend, she learned about a depression-prevention study at the University of Pittsburgh targeting older adults. Participants were split: one group received cognitive-behavioral therapy, while the other, including Carolyn, received dietary counseling. Guided by a social worker, she gradually replaced chips and cake with salmon, tuna, leafy greens, and other nutrient-rich options.
Fifteen months after the intervention, participants in both groups showed an astonishing 40–50% improvement in depressive symptoms, with only 8% developing major depression. Carolyn believed the transformation began with a fork—not a pill.
Science Meets Salad – The Rise of Nutritional Psychiatry: Carolyn’s story is emblematic of a profound shift in healthcare. Increasingly, scientists are uncovering how diet influences brain health, shaping everything from mood and memory to neurodevelopment and resilience. This movement—dubbed nutritional psychiatry—seeks to understand how food acts not just as fuel, but as a therapeutic agent for the mind.
And while causation can be hard to pin down—do healthy eaters also have better sleep and exercise habits, or does good food simply promote good feelings?—the evidence continues to build.
The Mediterranean Prescription: The best-supported brain diet today draws inspiration from traditional Mediterranean eating patterns, characterized by fresh produce, legumes, nuts, whole grains, olive oil, fish, and modest wine intake. This isn’t just cultural nostalgia—it is backed by science [1-3].
In the MILES trial, patients with moderate to severe depression who adopted a Mediterranean-style diet for 12 weeks saw significant improvements on the Montgomery-Åsberg Depression Rating Scale. Public health expert Almudena Sánchez-Villegas followed over 12,000 healthy Spaniards for six years, showing a 30% reduction in depression risk among those adhering to the diet. Her subsequent PREDIMED study linked the diet to even greater benefits—especially in people with diabetes, who saw a 40% reduction in depression risk [see Figure 1; Table 1].
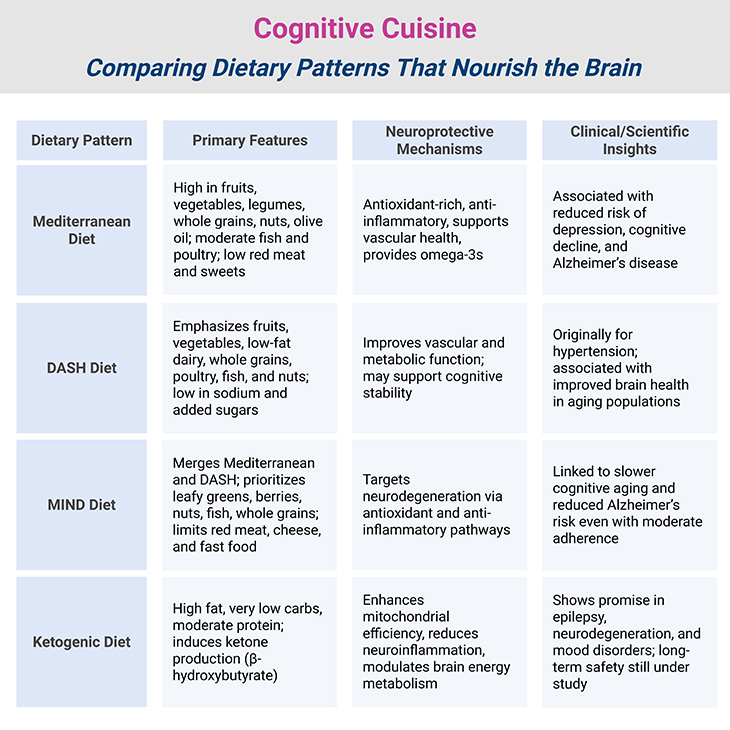
Table 1. Cognitive Cuisine: Comparing Dietary Patterns That Nourish the Brain
Junk Food – Shrinking Brains: Not all diets nourish. The Western dietary pattern—rich in sugar, processed meats, fried foods, and saturated fats—has been linked to higher rates of depression, anxiety, and cognitive decline. In 2015, psychiatrist Felice Jacka found that older adults who followed a Western diet for four years developed a smaller left hippocampus, the brain’s memory center [4-5].
Chronic consumption of unhealthy food appears to drive low-grade inflammation, which affects both gut and brain. Inflammation, while essential for fighting infection, can become destructive when prolonged, playing a role in depression, schizophrenia, Alzheimer’s, and bipolar disorder [6-7].
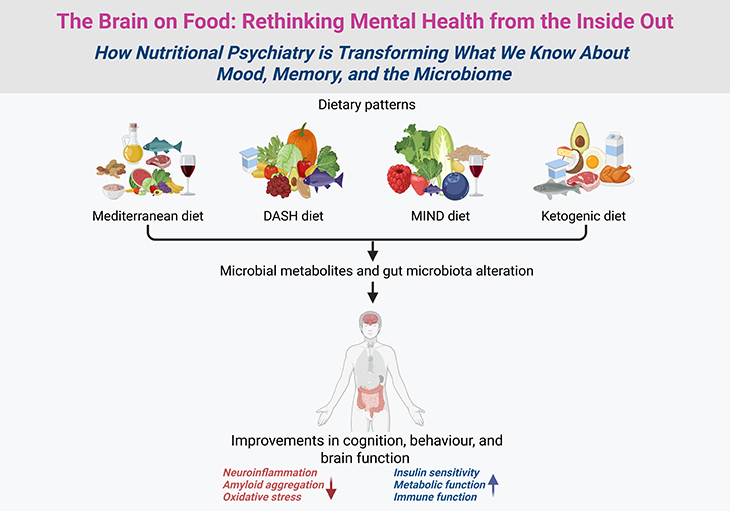
Gut Instinct – The Microbiome-Brain Connection: What we eat does not just nourish our bodies—it feeds the trillions of microbes residing in our gut. When diverse and balanced, this microbiome supports digestion, immunity, and serotonin production. But fast food and processed meals can devastate it (see Figure 1; Figure 2; and Table 2) [8-9].
In a 2014 experiment, university student Tom Spector subsisted on McDonald’s for 10 days, wiping out one-third of his gut’s microbial species—and feeling markedly worse. More alarmingly, inflammation in the gut diverts tryptophan, a serotonin precursor, into a metabolic route that creates neurotoxic compounds linked to depression and neurodegenerative diseases [10].
Reversing the Damage – The Diet Swap Experiment: But the good news is also rapid: in a 2015 University of Pittsburgh study, 20 African-Americans and 20 rural South Africans swapped diets. After two weeks, Americans on a fiber-rich African diet showed reduced inflammation and a 250% spike in butyrate-producing bacteria—microbes that protect against cancer. The South Africans, conversely, showed worrying microbial shifts after consuming a Western-style diet.
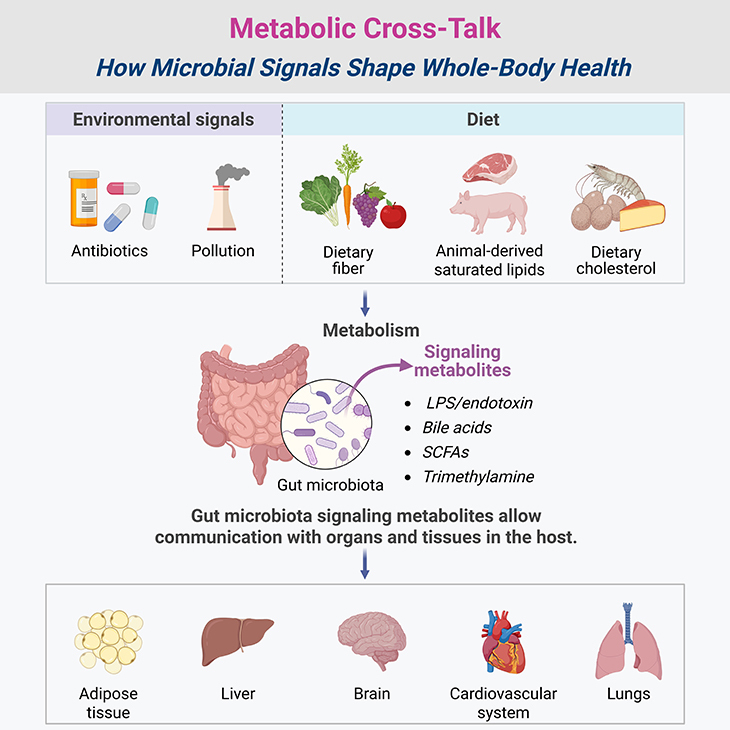
Figure 2. Metabolic Cross-Talk: How Microbial Signals Shape Whole-Body Health. Systemic metabolic regulation by gut microbiota: signaling pathways from the intestinal lumen to distant organs. (1) Metabolism is a dynamic, bidirectional process shaped by the gut microbiota, which continuously respond to environmental cues—particularly dietary inputs. These microbial communities ferment dietary macronutrients into bioactive metabolites such as short-chain fatty acids (SCFAs), secondary bile acids, indole derivatives, and lipopolysaccharides (LPS). These compounds act as signaling molecules that influence host physiology by interacting with receptors and pathways in adipose tissue, liver, brain, cardiovascular system, and lungs. For example, SCFAs modulate insulin sensitivity, lipid metabolism, and appetite regulation via G-protein-coupled receptors, while microbial bile acid derivatives influence glucose homeostasis through FXR and TGR5 signaling. (2) Conversely, host metabolic states—such as obesity, fasting, or inflammation—can reshape microbial composition and function, creating a feedback loop that reinforces or disrupts metabolic balance. Dysbiosis, often driven by Western dietary patterns, reduces microbial diversity and promotes systemic inflammation via increased intestinal permeability and LPS translocation. This intricate cross-talk underscores the microbiota as a metabolic signaling hub, linking gut ecology to systemic health and disease susceptibility.
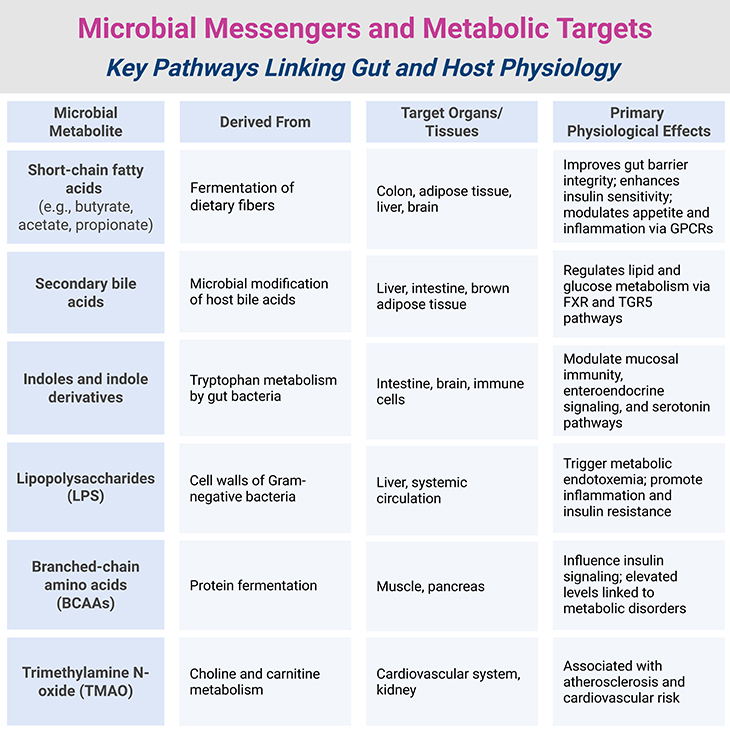
Table 2. Metabolic Cross-Talk: How Microbial Signals Shape Whole-Body Health
Clinicians Speak Out – Food as Frontline Medicine: Harvard psychiatrist Emily Deans believes diet is as important as any prescription. She discusses nutrition and meal timing with nearly all her patients, especially those battling depression and anxiety. She also cautions against overhyping probiotic supplements, urging instead a return to whole foods—rich in fiber, fermented ingredients, and omega-3s (see Table 3).
Back to the Beginning – Evolution’s Clues: Human dietary patterns evolved out of necessity. Around 160,000 years ago, during a harsh glacial period, early humans likely survived by exploiting coastal shellfish beds—reliable sources of omega-3 fatty acids, especially docosahexaenoic acid (DHA) [11-12].
DHA, which comprises a significant portion of neuronal cell membranes, facilitates communication between brain cells and boosts brain-derived neurotrophic factor (BDNF), a protein essential for neuron survival. Psychiatrist Michael A. Crawford has argued for decades that DHA from seafood was instrumental in human brain evolution—and that our modern departure from marine-based nutrition may be fueling today’s mental health crisis.
A New Pillar of Psychiatry: In 2015, the International Society for Nutritional Psychiatry Research, co-founded by Jacka, published a report in The Lancet Psychiatry, urging nutrition’s inclusion in mainstream psychiatric care. The authors emphasized that diet is as relevant to psychiatry as it is to cardiology, endocrinology, or gastroenterology—especially given the limited efficacy of many psychiatric drugs [13-14].
Selective serotonin reuptake inhibitors (SSRIs), for example, often perform no better than placebo in cases of mild to moderate depression. As research expands, nutrition-based treatments—safe, affordable, and evolutionarily sound—are poised to play a central role in psychiatric care.
Carolyn’s Closing Chapter—And Ours: Today, Carolyn lives by a simple truth: what you eat changes how you feel. Her story—and the science behind it—reminds us that food is far more than sustenance. It is a tool for healing, a foundation for resilience, and perhaps one of the most underutilized resources in mental health [14].
As we confront rising rates of depression, anxiety, dementia, and chronic illness, one thing is clear: the path to a healthier brain may well begin on our plates (see Figure 3; Table 3; and Table 4).
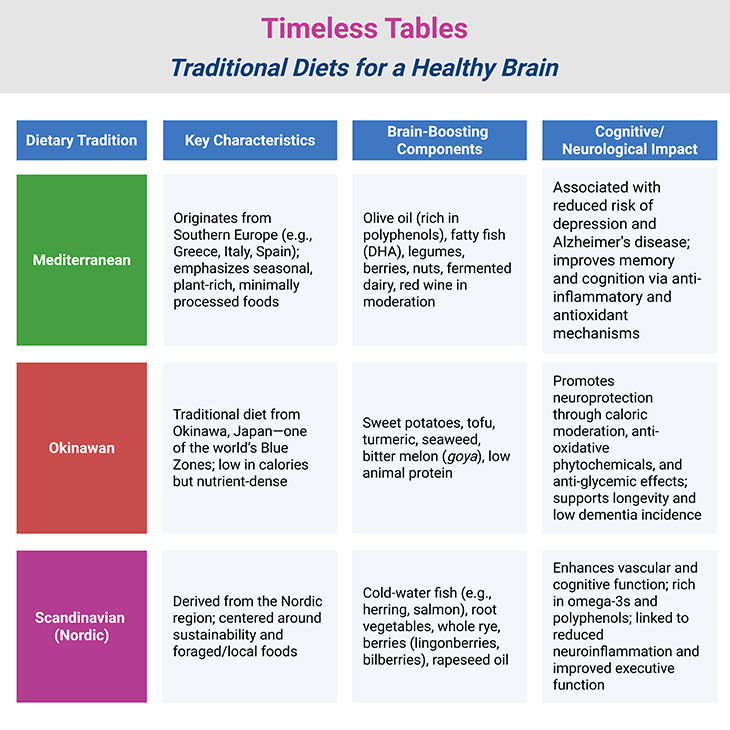
Table 3. Timeless Tables: Traditional Diets for a Healthy Brain.
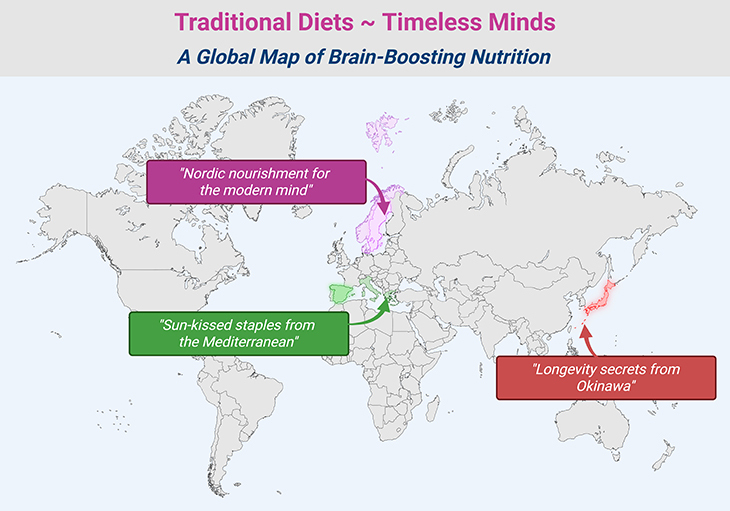
Figure 3. Traditional Diets, Timeless Minds: A Global Map of Brain-Boosting Nutrition.
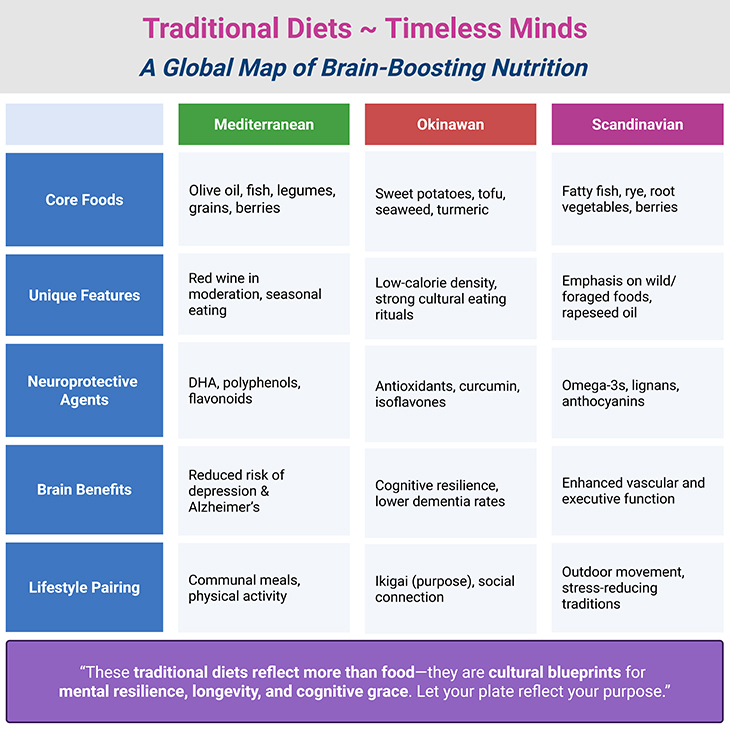
Table 4. Traditional Diets, Timeless Minds: A Global Map of Brain-Boosting Nutrition.
Take-Home Message
- Food is more than fuel—it is information that shapes how we think, feel, and age.
- Traditional diets, like the Mediterranean model, support cognitive resilience and emotional balance.
- Nutritional psychiatry is emerging as a credible, evidence-based field alongside conventional mental health care.
- Inflammation is a hidden culprit in many psychiatric conditions, and diet plays a key role in modulating it.
- A diverse, fiber-rich diet supports a healthy microbiome, which is essential for gut-brain communication.
- Nutrients like omega-3 fatty acids (DHA) are not optional—they are foundational to brain structure and function.
- Rapid dietary changes can shift the microbiome, for better or worse, in a matter of days.
- Whole foods outperform supplements—because the body recognizes nutrients in their natural state.
- Mental health is not just in our heads—it is also on our plates.
Summary and Conclusions
A Nutritional Renaissance for the Mind: In reimagining brain health through the lens of food, we uncover a story as ancient as evolution and as urgent as today’s mental health crisis. The mounting body of evidence—from interventional studies like SMILES and MILES to observational data from cohorts like PREDIMED—clearly signals that nutrition is not merely lifestyle advice, but a modifiable risk factor for psychiatric and cognitive disorders. Diets anchored in evolutionary wisdom, such as the Mediterranean and MIND diets, consistently show benefits in reducing depression risk, slowing cognitive decline, and enhancing emotional resilience.
Mechanistically, the impact is multidimensional. Omega-3 fatty acids, particularly DHA, support synaptic integrity, neuroplasticity, and anti-inflammatory signaling. Meanwhile, diets rich in polyphenols, antioxidants, fiber, and fermented foods feed a diverse and robust gut microbiome, which orchestrates serotonin synthesis and modulates the immune response. The inflammatory hypothesis of depression—once peripheral—is now central, with microglial overactivation, elevated cytokine levels, and disrupted tryptophan metabolism all under intense scrutiny. These findings are no longer speculative—they are corroborated across disciplines, from psychiatry and immunology to microbiology and neuroendocrinology.
Importantly, this narrative resists silver bullets. There is no “magic berry” or “miracle probiotic.” Instead, what emerges is a compelling framework: mental well-being is scaffolded by dietary patterns, not isolated nutrients. The sharp contrasts between brain-preserving traditional diets and inflammatory, ultra-processed Western fare highlight how our fork can be as mighty as our pharmacopoeia—if not mightier, for many.
As we confront stalled pharmaceutical pipelines and the limitations of current psychiatric drugs, nutrition offers a low-cost, accessible, and side-effect-free intervention that empowers patients as participants in their healing. For clinicians, this calls for a new model of care—one where psychiatrists consult alongside dietitians, and dietary history is as routine as medication review.
What began as Carolyn’s personal transformation is a clarion call for a broader medical awakening. If we are to meet the complexities of mental illness and neurodegeneration with equal complexity and compassion, we must begin where health begins: at the table.
For information on autism monitoring, screening and testing please read our blog.
References
Mediterranean Diet & Depression
- Parletta N, Zarnowiecki D, Cho J, Wilson A, Bogomolova S, Villani A, Itsiopoulos C, Niyonsenga T, Blunden S, Meyer B, Segal L, Baune BT, O’Dea K. A Mediterranean-style dietary intervention supplemented with fish oil improves diet quality and mental health in people with depression: A randomized controlled trial (HELFIMED). Nutr Neurosci. 2019 Jul;22(7):474-487. doi: 10.1080/1028415X.2017.1411320. Epub 2017 Dec 7. PMID: 29215971.
https://pubmed.ncbi.nlm.nih.gov/29215971/ - Sánchez-Villegas A, Delgado-Rodríguez M, Alonso A, Schlatter J, Lahortiga F, Serra Majem L, Martínez-González MA. Association of the Mediterranean dietary pattern with the incidence of depression: the Seguimiento Universidad de Navarra/University of Navarra follow-up (SUN) cohort. Arch Gen Psychiatry. 2009 Oct;66(10):1090-8. doi: 10.1001/archgenpsychiatry.2009.129. PMID: 19805699.
https://pubmed.ncbi.nlm.nih.gov/19805699/ - Martínez-Lapiscina EH, Clavero P, Toledo E, Estruch R, Salas-Salvadó J, San Julián B, Sanchez-Tainta A, Ros E, Valls-Pedret C, Martinez-Gonzalez MÁ. Mediterranean diet improves cognition: the PREDIMED-NAVARRA randomised trial. J Neurol Neurosurg Psychiatry. 2013 Dec;84(12):1318-25. doi: 10.1136/jnnp-2012-304792. Epub 2013 May 13. PMID: 23670794.
https://pubmed.ncbi.nlm.nih.gov/23670794/
Western Diet & Brain Structure
- Jacka FN, Cherbuin N, Anstey KJ, Sachdev P, Butterworth P. Western diet is associated with a smaller hippocampus: a longitudinal investigation. BMC Med. 2015 Sep 8;13:215. doi: 10.1186/s12916-015-0461-x. PMID: 26349802; PMCID: PMC4563885.
https://pubmed.ncbi.nlm.nih.gov/26349802/
- Jacka FN, Pasco JA, Mykletun A, Williams LJ, Hodge AM, O’Reilly SL, Nicholson GC, Kotowicz MA, Berk M. Association of Western and traditional diets with depression and anxiety in women. Am J Psychiatry. 2010 Mar;167(3):305-11. doi: 10.1176/appi.ajp.2009.09060881. Epub 2010 Jan 4. PMID: 20048020.
https://pubmed.ncbi.nlm.nih.gov/20048020/
Inflammation & Psychiatric Disorders
- Dowlati Y, Herrmann N, Swardfager W, Liu H, Sham L, Reim EK, Lanctôt KL. A meta-analysis of cytokines in major depression. Biol Psychiatry. 2010 Mar 1;67(5):446-57. doi: 10.1016/j.biopsych.2009.09.033. Epub 2009 Dec 16. PMID: 20015486.
https://pubmed.ncbi.nlm.nih.gov/20015486/
- Miller AH, Raison CL. The role of inflammation in depression: from evolutionary imperative to modern treatment target. Nat Rev Immunol. 2016 Jan;16(1):22-34. doi: 10.1038/nri.2015.5. PMID: 26711676; PMCID: PMC5542678.
https://pubmed.ncbi.nlm.nih.gov/26711676/
Microbiome & Mental Health
- Foster JA, McVey Neufeld KA. Gut-brain axis: how the microbiome influences anxiety and depression. Trends Neurosci. 2013 May;36(5):305-12. doi: 10.1016/j.tins.2013.01.005. Epub 2013 Feb 4. PMID: 23384445.
https://pubmed.ncbi.nlm.nih.gov/23384445/
- Cryan JF, O’Riordan KJ, Cowan CSM, Sandhu KV, Bastiaanssen TFS, Boehme M, Codagnone MG, Cussotto S, Fulling C, Golubeva AV, Guzzetta KE, Jaggar M, Long-Smith CM, Lyte JM, Martin JA, Molinero-Perez A, Moloney G, Morelli E, Morillas E, O’Connor R, Cruz-Pereira JS, Peterson VL, Rea K, Ritz NL, Sherwin E, Spichak S, Teichman EM, van de Wouw M, Ventura-Silva AP, Wallace-Fitzsimons SE, Hyland N, Clarke G, Dinan TG. The Microbiota-Gut-Brain Axis. Physiol Rev. 2019 Oct 1;99(4):1877-2013. doi: 10.1152/physrev.00018.2018. PMID: 31460832.
https://pubmed.ncbi.nlm.nih.gov/31460832/
Tryptophan Metabolism & Neurotoxicity
- Dantzer R. Role of the Kynurenine Metabolism Pathway in Inflammation-Induced Depression: Preclinical Approaches. Curr Top Behav Neurosci. 2017;31:117-138. doi: 10.1007/7854_2016_6. PMID: 27225497; PMCID: PMC6585430.
https://pubmed.ncbi.nlm.nih.gov/27225497/
DHA & Brain Evolution
- Crawford MA, Broadhurst CL, Guest M, Nagar A, Wang Y, Ghebremeskel K, Schmidt WF. A quantum theory for the irreplaceable role of docosahexaenoic acid in neural cell signalling throughout evolution. Prostaglandins Leukot Essent Fatty Acids. 2013 Jan;88(1):5-13. doi: 10.1016/j.plefa.2012.08.005. Epub 2012 Nov 30. PMID: 23206328.
https://pubmed.ncbi.nlm.nih.gov/23206328/
- Lauritzen L, Hansen HS, Jørgensen MH, Michaelsen KF. The essentiality of long chain n-3 fatty acids in relation to development and function of the brain and retina. Prog Lipid Res. 2001 Jan-Mar;40(1-2):1-94. doi: 10.1016/s0163-7827(00)00017-5. PMID: 11137568.
https://pubmed.ncbi.nlm.nih.gov/11137568/
Nutritional Psychiatry as a Field
- Sarris J, Logan AC, Akbaraly TN, Amminger GP, Balanzá-Martínez V, Freeman MP, Hibbeln J, Matsuoka Y, Mischoulon D, Mizoue T, Nanri A, Nishi D, Ramsey D, Rucklidge JJ, Sanchez-Villegas A, Scholey A, Su KP, Jacka FN; International Society for Nutritional Psychiatry Research. Nutritional medicine as mainstream in psychiatry. Lancet Psychiatry. 2015 Mar;2(3):271-4. doi: 10.1016/S2215-0366(14)00051-0. Epub 2015 Feb 25. PMID: 26359904.
https://pubmed.ncbi.nlm.nih.gov/26359904/
- Stetka B. Navigating Anxiety & Depression: The Best Diet for Your Brain. Sci Am. Mar 1, 2016
https://www.scientificamerican.com/