Table of Contents
- Introduction
- Unveiling Childhood Depression: Early Signs and Solutions
- Key Findings
- Navigating the Storm: Understanding Depression in Adolescence
- Key Triggers and Risk Factors
- Long-Term Implications
- Beyond the Baby Blues: Tackling Postnatal Depression and Psychosis
- Men and Depression: Breaking the Silence
- Risk Factors for Depression in Men
- The Complex Relationship Between Physical Illness and Depression
- Integrated Treatment Approaches
- Take-Home Messages
- Summary and Conclusions
- Did You Know About Folate Receptor Autoantibodies (FRAAs) and Brain Development?
- References
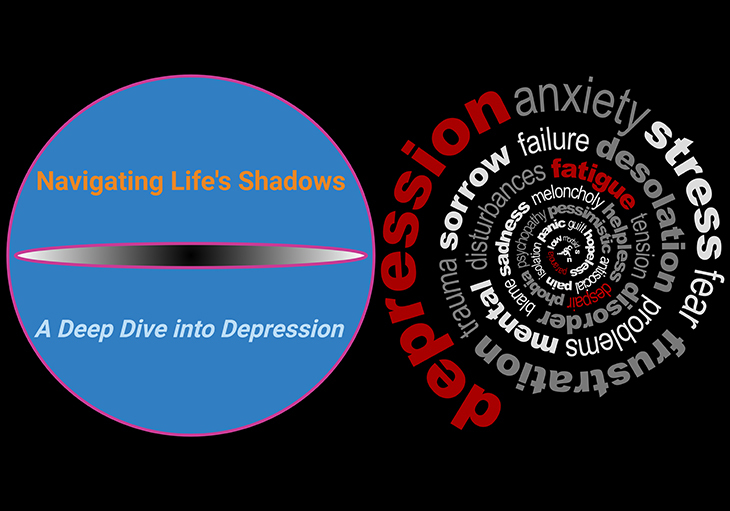
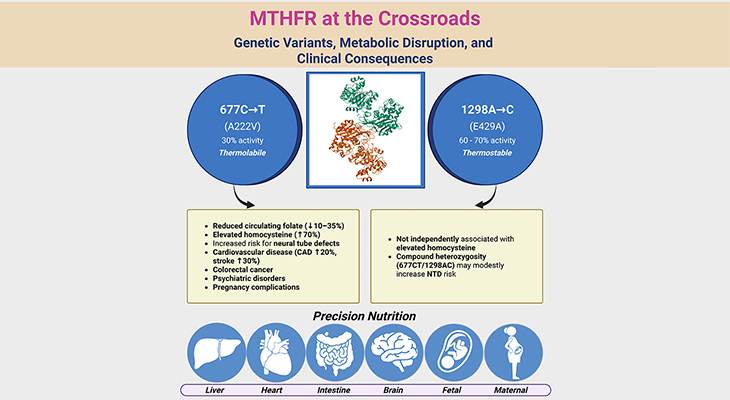
Figure 1. Navigating Life’s Shadows – A Deep Dive into Depression. Depression can affect individuals at various stages of life, each presenting unique risk factors and symptoms. From childhood and adolescence to adulthood, including postnatal challenges for women and specific issues for men, its complexity calls for early detection, personalized care, and integrated approaches that address the interplay between mental and physical health. For example: 1. Childhood: Depression is relatively uncommon in children under 11, but those with a family history of depression are four times more likely to experience it. 2. Adolescence: The prevalence of depression in adolescents is similar to that in older adults, with a significant increase during puberty. Adolescents aged 18-25 have the highest prevalence of major depressive episodes at 18.6%. 3. Adulthood: An estimated 21.0 million U.S. adults had at least one major depressive episode in 2021, representing 8.3% of all adults. The prevalence is higher among females (10.3%) compared to males (6.2%). 4. Postnatal Depression: Affects approximately 10-15% of new mothers, with significant implications for both mother and child. 5. Puerperal Psychosis: A rare but severe condition, occurring in about 1 in 1,000 pregnancies. 6. Men: Depression rates in men are often underreported, but life events such as unemployment and chronic physical health problems are significant risk factors. The prevalence of depression in individuals with chronic physical diseases is almost three times higher than those without such conditions. These statistics emphasize the widespread impact of depression across different life stages and the importance of addressing this pervasive issue through informed and compassionate care. [National Institute of Mental Health (NIMH): https://www.nimh.nih.gov/health/statistics/major-depression?form=MG0AV3; OASH Office on Women’s Health: https://womenshealth.gov/TalkingPPD]; Centers for Disease Control and Prevention (CDC): https://www.cdc.gov/mmwr/volumes/72/wr/mm7224a1.htm?form=MG0AV3] [1]
Introduction
Exploring Depression Across the Lifespan: Depression is a complex and pervasive mental health issue that can affect individuals at different stages of life, from childhood to old age. Understanding the nuances of depression at various life stages is crucial for early identification, effective intervention, and comprehensive support. This article delves into the multifaceted nature of depression, beginning with its manifestations in children and adolescents, moving through the challenges faced by women of childbearing age, and addressing the specific experiences of men, especially when depression coexists with physical health problems.
We explore how childhood depression was once thought to be non-existent and how research over the past few decades has challenged this belief, revealing the significant impact of depressive disorders on young children. In adolescents, the hormonal changes of puberty play a critical role in the onset of depression, with unique triggers and risk factors influencing its development.
For women of childbearing age, the focus shifts to two specific disorders related to childbirth: (i) postnatal depression and (ii) puerperal psychosis. These conditions not only affect the mother’s well-being but also have profound implications for the care and bonding with their newborns. Addressing these issues early is essential for the health of both mother and child.
In men, depression has often been underrecognized, leading to delays in seeking help and treatment. Understanding the unique ways in which men express and cope with depression, as well as the impact of life events and physical health problems, is key to improving mental health outcomes for this population. By examining depression across the lifespan (see Figure 1), we aim to shed light on the diverse experiences and challenges faced by individuals at different ages. Our goal is to provide a comprehensive understanding of depression, highlighting the importance of early detection, tailored interventions, and integrated treatment approaches to support mental health and well-being for all.
Unveiling Childhood Depression: Early Signs and Solutions
Childhood: For a long time, it was believed that depression was primarily an issue for middle-aged and older adults, and that children and adolescents were somehow immune to it. Those who suggested otherwise had little research to support their claims, as studies typically focused on individuals over the age of 18 (see Figure 2).
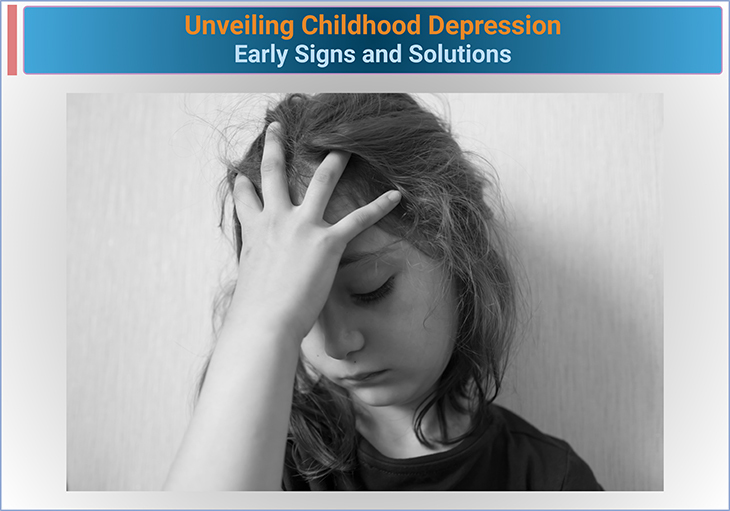
Figure 2. Unveiling Childhood Depression – Early Sings and Solutions. Understanding Depression in Children: Depression in children is a serious mental health condition that affects their emotional, social, and cognitive development. It is characterized by persistent feelings of sadness, hopelessness, and a lack of interest in activities that were once enjoyable. Unlike occasional mood swings, depression in children can interfere with their daily functioning and overall well-being. Key Facts About Depression in Children: 1. Prevalence: Approximately 4% of children aged 3-17 years in the United States have been diagnosed with depression. 2. Symptoms: Common symptoms include persistent sadness, irritability, changes in appetite or weight, difficulty sleeping, fatigue, and difficulty concentrating. 3. Risk Factors: Factors that increase the risk of depression in children include a family history of depression, exposure to trauma or stress, chronic medical conditions, and other mental health disorders such as anxiety. 4. Diagnosis: Depression in children is diagnosed through a comprehensive evaluation by a healthcare provider, which may include interviews, questionnaires, and observations. 5. Treatment: Treatment options for childhood depression often include a combination of psychotherapy (such as cognitive-behavioral therapy, CBT), medication, and support from family and school. Epidemiological Data: 1. Prevalence Rates: According to data from the Centers for Disease Control and Prevention (CDC), 4% of children aged 3-17 years have been diagnosed with depression. 2. Gender Differences: Depression is more commonly diagnosed in females (6%) compared to males (3%) in the same age group. 3. Co-occurring Conditions: Depression often co-occurs with other mental health conditions. For example, 37% of children with a current mental health condition have two or more conditions. 4. Treatment Access: Among children with depression, 79% received treatment or counseling from a mental health professional in the past year. Conclusion: Depression in children is a significant public health concern that requires early identification and intervention. Understanding the established facts and epidemiological data can help parents, educators, and healthcare providers support children who may be struggling with this condition.
However, starting around 1975, mental health researchers began to question this belief and initiated long-term studies to track children and adolescents over several years. These studies aimed to determine how many children experienced depression, had recurrent episodes, developed other mental health issues, or had only one depressive episode without further problems. The findings from these studies provided valuable insights into the risk and protective factors associated with childhood depression and highlighted differences in how depression manifests in boys and girls before and after puberty.
Key Findings
- Depression in Children Under 11: Depression is relatively uncommon in children under the age of 11. Interestingly, some studies suggest that boys may experience depression more frequently than girls at this age. Depression in children often co-occurs with anxiety or irritability and is rarely the first mental health issue they face. Many children with depression also struggle with conditions such as autism or disruptive behavior, and the stress from these conditions can lead to what is termed ‘exhaustion syndrome,’ which mirrors depressive symptoms.
- Family History: Children with a family history of depression are four times more likely to experience it themselves and are at a higher risk for recurrent episodes.
The recognition that children can indeed experience depression has introduced new challenges, particularly in terms of treatment. Many clinicians are cautious about prescribing medications designed for adults to younger individuals. Instead, talking therapies such as cognitive-behavioral therapy (CBT) and family-based approaches have shown promise. Recently, there has been a push to enhance children’s resilience to prevent depression, which includes integrating mental health education into school curricula and introducing ‘social-emotional learning’ (SEL) classes. Programs focusing on mindfulness for children are also being explored as preventive measures [1-2].
Navigating the Storm: Understanding Depression in Adolescence
Adolescence: Anyone who has spent time with an adolescent knows that their moods, sleep habits, and self-esteem can change rapidly. It is common for teenagers to experience intense distress, making it challenging to distinguish between normal adolescent mood swings and clinical depression that needs treatment. Recent research, however, indicates that depression rates among adolescents are similar to those in older adults.
One significant finding from adolescent depression research is that puberty, rather than chronological age, triggers a notable increase in depression cases. This suggests that hormonal changes play a crucial role, as post-pubertal depression rates are twice as high in young women compared to young men. Adolescents with a family history of depression or bipolar disorder are at a higher risk of developing depression in early adulthood, with recurrent episodes often linked to family history (see Figure 3).
Key Triggers and Risk Factors
- Life Events: Adolescents face many normal life events that can trigger depression, such as peer group issues, relationship breakdowns, leaving home, and exposure to drugs and alcohol. Those with a family history of mood disorders are particularly vulnerable. Academic and economic pressures, like being unemployed or out of education (termed NEETs), also play a significant role. NEETs report depression rates three to five times higher than their peers, highlighting the need for comprehensive treatment approaches that address social and academic re-engagement.
- Treatment Ambivalence: Adolescents often feel ambivalent about taking medication for depression, and young men may find it difficult to engage with talking therapies. Solutions include activity and behavior-oriented groups and web-based programs. In Australia, research is exploring offering these options to all school pupils in critical academic years, aiming to prevent depression by addressing stressors early.
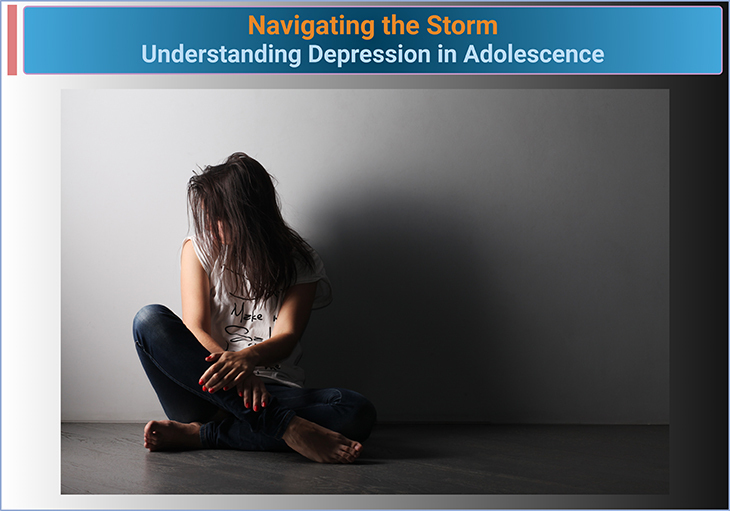
Figure 3. Navigating the Storm – Understanding Depression in Adolescence. Understanding Depression in Adolescence: Depression in adolescence is a significant mental health concern that can impact a teenager’s emotional, social, and academic life. It is characterized by persistent feelings of sadness, hopelessness, and a lack of interest in activities that were once enjoyable. Adolescents with depression may experience changes in their behavior, mood, and overall functioning. Key Facts About Depression in Adolescence: 1. Prevalence: Approximately 13% of adolescents aged 12-17 years in the United States have experienced at least one major depressive episode in the past year. 2. Symptoms: Common symptoms include persistent sadness, irritability, changes in appetite or weight, difficulty sleeping, fatigue, difficulty concentrating, and thoughts of death or suicide. 3. Risk Factors: Factors that increase the risk of depression in adolescents include a family history of depression, exposure to trauma or stress, chronic medical conditions, and other mental health disorders such as anxiety. 4. Diagnosis: Depression in adolescents is diagnosed through a comprehensive evaluation by a healthcare provider, which may include interviews, questionnaires, and observations. 5. Treatment: Treatment options for adolescent depression often include a combination of psychotherapy (such as cognitive-behavioral therapy, CBT), medication, and support from family and school. Epidemiological Data: 1. Prevalence Rates: According to data from the National Surveys on Drug Use and Health, the percentage of adolescents who experienced one or more major depressive episodes in the previous 12 months increased from 9% in 2005 to 13% in 2016. 2. Gender Differences: Depression is more commonly diagnosed in females compared to males in the adolescent age group. 3. Co-occurring Conditions: Depression often co-occurs with other mental health conditions. For example, adolescents with depression may also experience anxiety, behavioral disorders, or substance use disorders. 4. Treatment Access: Despite the high prevalence of depression, only about 40% of adolescents with severe impairment from depression receive treatment. Conclusion: Depression in adolescence is a critical public health issue that requires early identification and intervention. Understanding the established facts and epidemiological data can help parents, educators, and healthcare providers support adolescents who may be struggling with this condition.
Long-Term Implications
While many adolescents with depression find that their psychological issues are confined to this period, others may continue to struggle for years. Identifying those most likely to develop recurrent mood episodes is a key research priority. It is also essential to distinguish between those who may experience recurrent depression and those at risk of bipolar disorder, as 70% of individuals with bipolar disorder report a depressive episode during adolescence. However, identifying adolescents at risk of mania remains challenging due to behaviors like risk-taking and staying up all night, which are not necessarily signs of illness.
Currently, having a family history of bipolar disorder is one of the few indicators of future mania risk. Despite this, predicting bipolar disorder with certainty is difficult, making it impractical to prescribe adult treatments to at-risk adolescents. Researchers are focusing on interventions with a high benefit-to-risk ratio, such as lifestyle management and psycho-education programs, to help manage early symptoms and social issues without the side effects of medication. However, more evidence is needed to support these strategies in clinical practice [1-2].
Beyond the Baby Blues: Tackling Postnatal Depression and Psychosis
Depression in Women of Childbearing Age: Rather than addressing all forms of depression in women, this section focuses on two depressive disorders linked to childbearing: (i) postnatal depression and (ii) puerperal psychosis.
Postnatal Depression: The birth of a baby is usually a joyous event, so postnatal depression is often hard for outsiders to comprehend. It is common for new mothers to feel emotional or weepy right after giving birth due to hormonal changes and physical exhaustion. However, these “baby blues” differ from more severe and persistent postnatal depression, which requires urgent attention and treatment. Any intervention should address the mother’s feelings of guilt about her depression (see Figure 4; Box-1).

Figure 4. Beyond the Baby Blues – Tackling Postnatal Depression. Understanding Post-Natal Depression: Post-natal depression, also known as postpartum depression (PPD), is a type of depression that occurs after childbirth. It is more severe and long-lasting than the “baby blues,” which are common and typically resolve within two weeks. PPD can affect a mother’s ability to care for her baby and handle daily tasks. Key Facts About Post-Natal Depression: 1. Prevalence: Post-natal depression affects approximately 1 in 7 new mothers. 2. Symptoms: Symptoms of PPD include severe mood swings, excessive crying, difficulty bonding with the baby, withdrawal from family and friends, changes in appetite, sleep disturbances, overwhelming fatigue, and feelings of worthlessness or guilt. 3. Risk Factors: Factors that increase the risk of PPD include a history of depression or anxiety, family history of mental health disorders, stressful life events, lack of support, and complications during childbirth. 4. Diagnosis: PPD is diagnosed through a comprehensive evaluation by a healthcare provider, which may include interviews, questionnaires, and observations. 5. Treatment: Treatment options for PPD often include a combination of psychotherapy (such as cognitive-behavioral therapy, CBT), medication, and support from family and friends. Early intervention is crucial for effective treatment. Epidemiological Data: 1. Prevalence Rates: According to the Cleveland Clinic, PPD affects up to 15% of women after childbirth. 2. Types of Post-Natal Depression: There are three types of postpartum mood disorders: (a) baby blues, (b) postpartum depression, and (c) postpartum psychosis. Baby blues affect 50-75% of new mothers and usually resolve within two weeks. 3. Co-occurring Conditions: PPD can co-occur with other mental health conditions, such as anxiety and panic disorders. 4. Treatment Access: Many women with PPD do not seek treatment due to stigma and lack of awareness. Early intervention and support are essential for recovery. Conclusion: Post-natal depression is a significant mental health concern that requires awareness and understanding. Recognizing the signs and symptoms, along with understanding the epidemiological data, can help in providing the necessary support and treatment for new mothers struggling with this condition.
Postnatal depression shares many symptoms with other forms of depression but stands out due to its impact on the baby. It not only affects the mother’s self-care and quality of life but can also hinder her ability to care for her child. This condition can complicate breastfeeding, as some antidepressant medications pass through breast milk. Additionally, depression can disrupt the bonding process between mother and child, leading to feelings of inadequacy and prolonging the depression. Recognizing and treating this condition early is crucial for both the mother and the child.
Many clinical programs aim to identify and treat postnatal depression as early as possible, often using screening questionnaires in obstetric and midwifery services. Research has shown that depressive symptoms can start during pregnancy, challenging the notion that all expectant mothers are always happy. This finding underscores the need for earlier screening and support during pregnancy [3].
When a pregnant woman experiences depressive symptoms, her stress hormone system may become overactive. Since these hormones can cross the placenta, they might affect the baby’s stress responses, emphasizing the importance of treating depression during pregnancy and childbirth for both the short-term and long-term well-being of the mother and child [4-5].
Puerperal Psychosis: Puerperal or postpartum psychosis is a rare but severe condition that affects about one in 1,000 pregnancies. Related to bipolar disorder, it includes symptoms such as loss of reality, hallucinations, delusions, and thoughts of suicide or harming the baby. This condition has been recognized throughout history, with detailed descriptions dating back to the 18th century. Historical accounts often judged the condition harshly, linking it to deviations from expected female behavior and maternal duty.
Figure 5. Beyond the Baby Blues – Tackling Postpartum Psychosis. Understanding Postpartum Depression: Postpartum depression (PPD) is a type of depression that occurs after childbirth. It is more severe and long-lasting than the “baby blues,” which are common and typically resolve within two weeks. PPD can significantly impact a mother’s ability to care for her baby and handle daily tasks. Key Facts About Postpartum Depression: 1. Prevalence: Postpartum depression affects approximately 1 in 7 new mothers. 2. Symptoms: Symptoms of PPD include severe mood swings, excessive crying, difficulty bonding with the baby, withdrawal from family and friends, changes in appetite, sleep disturbances, overwhelming fatigue, and feelings of worthlessness or guilt. 3. Risk Factors: Factors that increase the risk of PPD include a history of depression or anxiety, family history of mental health disorders, stressful life events, lack of support, and complications during childbirth. 4. Diagnosis: PPD is diagnosed through a comprehensive evaluation by a healthcare provider, which may include interviews, questionnaires, and observations. 5. Treatment: Treatment options for PPD often include a combination of psychotherapy (such as cognitive-behavioral therapy, CBT), medication, and support from family and friends. Early intervention is crucial for effective treatment. Epidemiological Data: 1. Prevalence Rates: According to the Cleveland Clinic, PPD affects up to 15% of women after childbirth. 2. Types of Postpartum Depression: There are three types of postpartum mood disorders: (a) baby blues, (b) postpartum depression, and (c) postpartum psychosis. Baby blues affect 50-75% of new mothers and usually resolve within two weeks. 3. Co-occurring Conditions: PPD can co-occur with other mental health conditions, such as anxiety and panic disorders. 4. Treatment Access: Many women with PPD do not seek treatment due to stigma and lack of awareness. Early intervention and support are essential for recovery. Conclusion: Postpartum depression is a significant mental health concern that requires awareness and understanding. Recognizing the signs and symptoms, along with understanding the epidemiological data, can help in providing the necessary support and treatment for new mothers struggling with this condition.
Today, puerperal psychosis is considered a medical emergency, often requiring inpatient treatment in specialized mother and baby units. Confidential inquiries into maternal deaths, such as “Why Mothers Die,” reveal that suicide is the leading cause of death among new mothers and often involves mothers killing their children in a misguided attempt to save them from future suffering (see Figure 5; Box-1).
This historical and contemporary understanding highlights the need for early intervention and comprehensive care for new mothers experiencing severe mental health issues [4-6].
Box-1. Infanticide – The Overlooked Crisis of Peri-natal Depression and Puerperal Pschoses[9].
Men and Depression: Breaking the Silence
Depression in Men: Depression has often been labeled a “women’s disease,” but it’s becoming clear that men are affected too. Health campaigns are now targeting men to help identify depression early and encourage treatment. While men and women share similar depression symptoms, the way men express and react to these symptoms can differ. For example, men might become withdrawn instead of seeking support, may display hostility, and often use alcohol to cope. Additionally, men may struggle to accept they have a mental health issue, often denying it, delaying help, or refusing treatment altogether (see Figure 6) [7].
Risk Factors for Depression in Men
There are no unique causes of depression specific to men, but certain life events are strongly linked to its onset. Becoming unemployed, retiring, losing a partner, and changes in social roles are all risk factors. Chronic physical health problems or increasing disability can also trigger depression.
Figure 6. Men and Depression – Breaking the Silence. Understanding Depression in Men: Depression in men is a significant mental health issue that often goes unrecognized and untreated. Men may experience depression differently than women, and societal expectations can make it challenging for them to seek help. Recognizing the signs and symptoms is crucial for early intervention and treatment. Key Facts About Depression in Men: 1. Prevalence: Depression affects millions of men each year. It is estimated that over 6 million men in the United States experience depression annually. 2. Symptoms: Common symptoms of depression in men include persistent sadness, irritability, anger, fatigue, difficulty sleeping, changes in appetite, and loss of interest in activities. Men may also exhibit behaviors such as escapism, substance abuse, and risky activities. 3. Risk Factors: Factors that increase the risk of depression in men include a family history of depression, chronic medical conditions, significant life changes, and stress. Men may also be less likely to seek help due to societal expectations and stigma. 4. Diagnosis: Depression in men is diagnosed through a comprehensive evaluation by a healthcare provider, which may include interviews, questionnaires, and observations. 5. Treatment: Treatment options for depression in men often include a combination of psychotherapy (such as cognitive-behavioral therapy, CBT), medication, and lifestyle changes. Support from family and friends is also essential. Epidemiological Data: 1. Prevalence Rates: According to the Mayo Clinic, depression affects millions of men each year, with many cases going undiagnosed and untreated. 2. Gender Differences: Men are less likely to express sadness and more likely to exhibit irritability, anger, or aggression. This can make it challenging to recognize depression in men. 3. Co-occurring Conditions: Depression in men often co-occurs with other mental health conditions, such as anxiety and substance use disorders. 4. Treatment Access: Despite the prevalence of depression, many men do not seek treatment due to stigma and societal expectations. Early intervention and support are crucial for effective treatment. Conclusion: Depression in men is a critical public health issue that requires awareness and understanding. Recognizing the signs and symptoms, along with understanding the epidemiological data, can help in providing the necessary support and treatment for men struggling with this condition.
The Complex Relationship Between Physical Illness and Depression
The link between physical illness and depression is intricate. When people are depressed, they often feel their overall health is worse, and those who are ill or in pain may become depressed. Some medical conditions, like an under-functioning thyroid gland (hypothyroidism), can mimic depression symptoms. People with chronic physical diseases are nearly three times more likely to suffer from depression compared to those without these conditions. Depression is also linked to a higher risk of certain illnesses, such as coronary heart disease, stroke, some cancers, and certain types of diabetes. These findings are crucial because they suggest shared genetic risk factors between depression and these diseases [8].
Integrated Treatment Approaches
Recognizing the connection between physical health and depression, doctors and psychiatrists now understand that treating both the depression and the medical condition can improve outcomes. Many programs for managing chronic physical diseases now include strategies for addressing depression, highlighting the importance of integrated treatment approaches [1-3].
Take-Home Messages
Depression Affects All Ages
- Depression can occur at any stage of life, from childhood through old age, and it is important to recognize the signs and symptoms in each age group.
Childhood Depression
- Once thought to be non-existent, childhood depression has been recognized as a significant issue. It often occurs alongside other conditions like autism and requires early detection and intervention.
Adolescent Depression
- Puberty is a critical trigger for depression in adolescents, with hormonal changes and life stressors such as academic pressure and social changes playing significant roles. Early intervention and support are crucial.
Postnatal Depression and Puerperal Psychosis
- These conditions highlight the impact of depression on both mothers and their babies. Early detection and comprehensive care are vital for the health of both mother and child.
Depression in Men
- Often underrecognized, depression in men requires targeted health campaigns and support. Men may express and cope with depression differently, and acknowledging these differences is important for effective treatment.
Interconnectedness of Physical and Mental Health
- Depression is closely linked with physical health conditions, and integrated treatment approaches that address both mental and physical health are essential for improved outcomes.
Importance of Early Detection and Tailored Interventions
- Recognizing and addressing depression early, with tailored interventions, is key to supporting mental health and well-being across the lifespan.
These take-home messages emphasize the importance of understanding and addressing depression at various life stages, highlighting the need for comprehensive and compassionate care to promote mental health for all individuals.
(Cf. previous blogs entitled as: “Decoding Depression: Comprehensive Insights and Future Horizons.” “Demystifying Depression: The Biological Blueprints Behind the Blues.”)
Summary and Conclusions
Depression is a multifaceted mental health issue that can strike at any stage of life, from childhood through to old age. This article has explored the different manifestations of depression across the lifespan, emphasizing the unique challenges faced by children, adolescents, women of childbearing age, and men. In childhood, depression was long thought to be nonexistent until research in the mid-1970s revealed its significant impact, particularly when intertwined with other conditions like autism. Adolescence brings its own complexities, with puberty acting as a critical trigger for depression, compounded by life events and stressors such as academic pressures and social changes.
For women of childbearing age, postnatal depression and puerperal psychosis highlight the profound effects of depression on both mother and child, emphasizing the need for early detection and intervention. Men, often underrecognized in depression discussions, face unique challenges in expressing and addressing their symptoms, with life events and physical health problems acting as significant risk factors.
Overall, understanding the diverse experiences of depression across different life stages is crucial for early identification and effective support. Comprehensive, tailored, and integrated treatment approaches are essential to promoting mental health and well-being for individuals of all ages. The exploration of depression in its various forms underscores the importance of addressing this pervasive issue through informed and compassionate care.
For information on autism monitoring, screening and testing please read our blog.
References
- Lee B, Wang Y, Carlson SA, et al. National, State-Level, and County-Level Prevalence Estimates of Adults Aged ≥18 Years Self-Reporting a Lifetime Diagnosis of Depression — United States, 2020. MMWR Morb Mortal Wkly Rep 2023;72:644–650.
http://dx.doi.org/10.15585/mmwr.mm7224a1 - Zwolińska W, Dmitrzak-Węglarz M, Słopień A. Biomarkers in Child and Adolescent Depression. Child Psychiatry Hum Dev. 2023 Feb;54(1):266-281. doi: 10.1007/s10578-021-01246-y. Epub 2021 Sep 29. PMID: 34590201; PMCID: PMC9867683.
https://pubmed.ncbi.nlm.nih.gov/34590201/
- Marland H. Disappointment and desolation: women, doctors and interpretations of puerperal insanity in the nineteenth century. Hist Psychiatry. 2003 Sep;14(55 Pt 3):303-20. doi: 10.1177/0957154X030143003. PMID: 14621687.
https://pubmed.ncbi.nlm.nih.gov/14621687/ - O’Hara MW, McCabe JE. Postpartum depression: current status and future directions. Annu Rev Clin Psychol. 2013;9:379-407. doi: 10.1146/annurev-clinpsy-050212-185612. Epub 2013 Feb 1. PMID: 23394227.
https://pubmed.ncbi.nlm.nih.gov/23394227/
- Payne JL, Maguire J. Pathophysiological mechanisms implicated in postpartum depression. Front Neuroendocrinol. 2019 Jan;52:165-180. doi: 10.1016/j.yfrne.2018.12.001. Epub 2018 Dec 12. PMID: 30552910; PMCID: PMC6370514.
https://pubmed.ncbi.nlm.nih.gov/30552910/
- Dennerstein L, Soares CN. The unique challenges of managing depression in mid-life women. World Psychiatry. 2008 Oct;7(3):137-42. doi: 10.1002/j.2051-5545.2008.tb00180.x. PMID: 18836580; PMCID: PMC2559916.
https://pubmed.ncbi.nlm.nih.gov/18836580/
- Sloan DM, Sandt AR. Gender differences in depression. Womens Health (Lond). 2006 May;2(3):425-34. doi: 10.2217/17455057.2.3.425. PMID: 19803914.
https://pubmed.ncbi.nlm.nih.gov/19803914/
- Goldberg D. The detection and treatment of depression in the physically ill. World Psychiatry. 2010 Feb;9(1):16-20. doi: 10.1002/j.2051-5545.2010.tb00256.x. PMID: 20148148; PMCID: PMC2816927.
https://pubmed.ncbi.nlm.nih.gov/20148148/
- Hatters Friedman S, Sorrentino R. Commentary: postpartum psychosis, infanticide, and insanity–implications for forensic psychiatry. J Am Acad Psychiatry Law. 2012;40(3):326-32. PMID: 22960914.
https://pubmed.ncbi.nlm.nih.gov/22960914/